
Links Between Periodontal Disease and Systemic Health Issues
Maintaining good oral care is about more than just a healthy mouth. As a dental professional, you know that periodontitis, the chronic inflammatory disease that affects the tissues supporting the teeth, is tied to other issues in the body, which raises the importance of helping patients succeed.
But did you know just how broad the spectrum of associated issues is? Research shows that no fewer than 57 systemic conditions may be linked to periodontal diseases, and many of them may take your patients by surprise.

In this article, we’ll explore the many related health issues that have been scientifically connected with inflammatory periodontal diseases, while pointing you to helpful resources so you can provide for your patients to help them on the journey toward holistic well-being.
Inflammation and Periodontal Disease
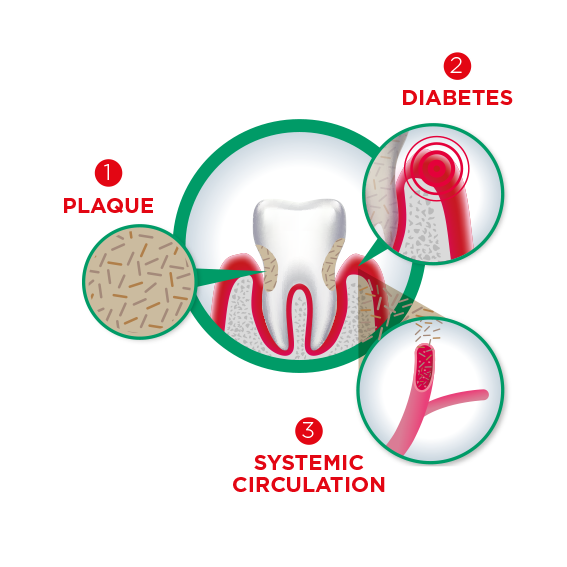
Inflammation is central to periodontal disease, triggered by the body’s response to periodontal pathogens in the biofilm. When the inflammatory response to bacterial infection becomes chronic, it causes damage to the supporting structures of the teeth (the root cementum, periodontal ligament and alveolar bone), causing the well-known process of bone loss and eventually even tooth loss.
But the impact and implications of periodontal inflammation are not necessarily limited to the mouth. As one example, microorganisms can travel from this area to other parts of the body, eliciting inflammatory responses at those sites. Furthermore, as we’ll explore, periodontal disease and the associated inflammation have been scientifically linked to a number of systemic health issues.
Links between periodontal disease and systemic health issues
From pregnancy issues to cardiovascular diseases to cancer, arthritis, diabetes, Alzheimer’s and beyond, research has discovered possible links between inflammatory periodontal disease and many prominent health issues that people hope to avoid. Here are a few that are particularly deserving of awareness.
Periodontitis and rheumatoid arthritis
The connection between chronic periodontitis and rheumatoid arthritis has been studied for many years, with a biological link between the two first postulated nearly 40 years ago. Over the past decade or so, evidence has begun to mount. A review by Clifton O. Bingham and Malini Monib published in 2015 noted that “A number of recent studies have evaluated the periopathogenic roles of Porphyromonas gingivalis, the oral microbiome, and mechanisms of site-specific and substrate-specific citrullination. These are helping to further elucidate the interactions between these two inflammatory disease processes.”
More recently, findings from a large cohort study reinforced that periodontitis is indeed associated with an increased risk of developing rheumatoid arthritis. A comprehensive review paper that looked at the literature about periodontitis and rheumatoid arthritis, published between 2012 and 2017, made some interesting observations, and to the authors, it was very clear the two diseases are strongly related. However, the way they are connected might not be as straightforward as you’d think. Although animal models provide some insight into plausible biological mechanisms – such as dissemination of periodontal pathogens – much remains unclear. So far, research has not really been able to establish causal relationships either, if such causality even exists.
It does, however, seem that a specific subset of patients is susceptible for both diseases, and once they occur, they seem to be connected intimately.
One 2019 study even found that the significant association between periodontitis and rheumatoid arthritis was even more evident and pronounced in patients with more severe cases of both diseases.
Although the biggest challenge is to identify this subset of patients as early as possible, inflammation is likely the common denominator that unifies them as a group. And this is also the mechanism that might help you to talk about this relationship with your patients.
Periodontal disease and pregnancy
The relationship between pregnancy and an increased risk of periodontal disease already gained attention as early as the 1960s. Suspected by empirical observations and confirmed by research, pregnant women are more likely to develop gingivitis, with an estimated prevalence of 30 to 100 percent.
The reason for the increased inflammatory response is thought not to be the presence of periodontal bacteria per se, but the elevated levels of several hormones, including estrogen, progesterone, and estradiol, influencing the host response. The prominence of so-called “pregnancy gingivitis” serves as an impetus for pregnant women to place an even stronger focus on oral care during this vital time.
When talking about pregnancy and periodontal disease, the term “bi-directional relationship” is mentioned frequently. Indeed, periodontal disease can have a negative impact on pregnancy outcomes. Although the first studies already date back a few decades, a joint consensus report published in 2013 by the American Academy of Periodontology and the European Federation in Periodontology proved eye-opening for the global medical community, suggesting that periodontal infections may increase the risk of pregnancy complications and adverse pregnancy outcomes. These can include preterm births, low birth weights, pre-eclampsia, and even miscarriages.
In an attempt to elucidate the mechanisms behind this relationship, early studies suggested that fetuses with a high antibody response against periodontal pathogens may have an increased risk for premature birth or low birth weight. Indirectly, this also implies that these pathogens can enter the bloodstream and travel as far as the uterus.
Indeed, there is strong evidence that periodontal pathogens can disseminate to the fetal-placental unit, causing local inflammation or even infecting the fetus directly. The fact that this does not always happen when periodontal pathogens are detected in the fetal-placental unit indicates that, again, the host immune response plays a central role.
Interestingly, small-scale treatment studies demonstrated that treatment of periodontitis in pregnant women may even reduce the risk for adverse pregnancy outcomes.
Most large RCTs have failed to reproduce these results, but most likely, the main reason for this was the timing of the interventions, usually taking place in the second trimester and onwards, when the periodontal pathogens may have already reached the fetal-placental unit. This emphasises the need for early intervention, or even better, prevention, perhaps as soon as the preconception period.
If you want to know more about the relationship between pregnancy and oral health, check out a recent webinar with international experts Dr. Phoebus Madianos and Dr. Mia Geisinger, hosted by SUNSTAR.
Periodontitis and diabetes risk
The link between periodontitis and diabetes is among the more well recognised and better understood among systemic health issues. Like the relationship between pregnancy and periodontitis mentioned above, this association is bi-directional.
Diabetes is a known risk factor for the development, progression, and severity of periodontitis. Already in the early 1990s, periodontitis assumed a spot on the list of chronic diabetic complications, and since then, it’s commonly accepted as the sixth complication of diabetes mellitus.
And for a reason: the mechanisms by which diabetes affects periodontal health shows many similarities with those of other chronic diabetic complications, such as cardiovascular disease, nephropathy, neuropathy and retinopathy. These complications are the result of damage to the large and/or small blood vessels, and are mainly driven by inflammation.
The same seems to be true for periodontitis. Because of the metabolic disturbances that characterise diabetes, the host immune response to periodontal pathogens seems to be even more exaggerated. This situation – often described as a hyper-inflammatory state – initiates and exacerbates the destructive processes that cause periodontal tissue breakdown.
This hyper-inflammatory state is also the starting point of the other direction of the association. As it happens, periodontitis can have a negative impact on the so-called metabolic control of patients with diabetes, meaning that the blood glucose levels are out of balance. Poor metabolic control is the most important cause of the chronic complications we mentioned above. Hence, indirectly, periodontitis increases the risk for diabetic complications. Besides this, poorly controlled blood glucose is a risk factor for progression of periodontal inflammation, meaning that without intervention, these patients end up in a vicious cycle. There is some evidence that periodontitis might even contribute to the development of new cases of diabetes. Again, inflammation is pivotal, since it has a direct effect on insulin resistance, a phenomenon that causes blood glucose levels to rise.
The two-way nature of this relationship creates all the more urgency for a strong preventative strategy, both for those who have diabetes or are at risk. There is considerable evidence that this is worth it.
For example, a study supported by SUNSTAR demonstrated that the dental setting is a feasible setting to detect a considerable amount of undiagnosed (pre)diabetes cases. The results of a large population-based cohort suggested that improving oral hygiene habits could lower the risk of developing diabetes. Another SUNSTAR-supported research project published in a leading primary care journal showed that extra attention to oral health can improve the quality of life of patients with diabetes.
The relationship between periodontitis and diabetes can have implications for your daily practice as a healthcare professional in many ways.
Check out these two videos.
Periodontitis and cardiovascular disease
Cardiovascular disease (CVD) is the leading cause of death in the world, and accounts for an estimated 45% of deaths in Europe. It’s a health issue that stands out on everyone’s radar. Cardiovascular disease has been connected to inflammatory periodontal issues.
A systematic review and meta-analysis published in 2020 “demonstrated modest but consistently increased risk of CVD in PD populations.” This is in line with observations from other studies over the past few decades. Recently, the European Federation of Periodontology (EFP) and the World Heart Federation (WHF) published a joint consensus report, which concluded that there is strong and convincing evidence for a significant association between periodontitis and CVD.
The central process underlying CVD is atherosclerosis, in which the arteries become clogged because of the formation of atheromatous plaque. The pathogenic pathways that cause atherosclerosis show striking resemblances with those underlying periodontal disease. Inflammation is at the basis again, this time both directly and indirectly. As mentioned before, there is strong evidence that periodontal pathogens can enter the bloodstream and travel to distant sites, also known as bacteremia.
These pathogens are also found in atherosclerotic plaques of patients with CVD, where most likely contribute to the inflammatory processes that cause the formation of these plaques. Indirectly, periodontal inflammation may also increase systemic levels of inflammatory mediates and cytokines, further enhancing the process of atherosclerosis.
Periodontal disease as a possible cause for Alzheimer’s
Another association that received a lot of media attention, reaching as far as the New York Times, is the one between periodontitis and Alzheimer’s disease. The famous newspaper reported on a study that showed that the relative risk for dementia was 22% higher in patients with severe periodontal inflammation and 26% higher in toothless patients, even after correcting for confounding factors such as age and smoking.
These findings were confirmed in a comprehensive literature review published in 2020. Although there is an urgent need for methodologically sound, longitudinal studies, the review by Kamer et al. concluded that “periodontal disease, through its inflammatory and bacterial burdens, could be ‘a biologically plausible risk factor’ for Alzheimer's disease.”
Periodontal disease and cancer
Cancer is a broad term encompassing many different forms.
A study published a couple of years ago in Oxford’s Journal of the National Cancer Institute “found a 24 percent increase in the relative risk of developing cancer among participants with severe periodontitis, compared to those with mild to no periodontitis.” The highest risk observed was for lung cancer, followed by colorectal cancer.
Although the association was not deemed strong enough to merit screening for particular cancers based on a periodontitis diagnosis, “we see a modest to moderate risk increase in cancer that seems to be holding up across studies, so perhaps dentists should say to their patients that there are risks related to periodontal disease, and this is one of them,” said Elizabeth Platz, Sc.D., deputy chair of the department of epidemiology at the Johns Hopkins Bloomberg School of Public Health.
Some evidence points to inflammation and periodontal microorganisms when talking about how periodontal disease may be associated with an increased risk for certain cancers. However, this mainly concerns small-scale, experimental studies, highlighting that there is an urgent need for more research.
Periodontal disease and respiratory issues
A consensus report on the association between periodontal diseases and cardiovascular diseases, diabetes and respiratory diseases published in March 2023 found that periodontitis is independently associated with cardiovascular diseases, diabetes, chronic obstructive pulmonary disease (COPD), obstructive sleep apnea and COVID-19 complications.
This report also examined several studies advancing multiple theories on the mechanisms underpinning the relationship between respiratory diseases and periodontitis. Likely theories include:
- Oral microorganisms can be aspirated along with oral secretions, which can exacerbate pulmonary inflammation and endothelial dysfunction (Hasegawa et al., 2014; Imai et al., 2021).
- Modifications of the oral and dental plaque/biofilm that occur with periodontitis (Wu et al., 2017).
- The low-grade inflammation associated with periodontitis
- The impact of cytokines on pulmonary epithelial cells
Finally, the report also notes that periodontitis and respiratory diseases share some common risk factors, including smoking, obesity and diabetes, that should be considered to decipher the underlying biological mechanisms involved in the association.
Periodontal disease and obesity
In a 2017 systematic review, 28 epidemiological studies and controlled clinical trials identified an association between obesity and an increased risk of periodontal disease.
The systematic review did not find conclusive evidence to explain the underlying mechanism behind the association it confirmed, but it did note that “the development of insulin resistance as a consequence of a chronic inflammatory state and oxidative stress could be implicated in the association between obesity and periodontitis”. A publication from 2020 provided a comprehensive overview of plausible mechanisms that how obesity may increase the risk for periodontal disease, including inflammation and immunodeficiency, impaired micro-circulation, microbial dysbiosis, hyposalivation and/or xerostomia, and psychosocial factors. Periodontitis conversely may also increase the risk for obesity, again by means of inflammation, nutritional factors, tooth loss, psychosocial factors, changes to the gut microbiome, and other unknown factors. Finally, many risk factors are identified that are shared between the two conditions, such as genetics/epigenetics, socio-economic status, lifestyle factors, and aging.
Periodontal disease and kidney disease
A study published in 2023 confirmed the bidirectionality of the relationship between periodontal disease and kidney disease.
Though the causality of the relationship between periodontitis and kidney disease has not been substantially identified, a 2021 study advanced and substantiated several associations: factors affecting the bidirectional relationship may include how periodontal disease affects the oral flora of its carriers, how it impacts various proinflammatory mediators that are also associated with a risk of kidney disease, such as IL-1 IL-6, IL-8. IL-17, and TNF-α, and the increase in oxidative stress produced by periodontal disease.
Periodontal disease and inflammatory bowel diseases
Recent studies on the relationship between inflammatory bowel disease (IBD) and periodontal disease have shown that patients with IBDs also face an increased risk of periodontal diseases because the diseases modify their oral microbiota and inflammatory processes.
Read our blog dedicated to the Latest Research on the Connection Between Inflammatory Bowel Diseases and Oral Health.
Indeed, an EFP publication also mentions that there are multiple similarities between periodontitis and IBD with respect to their pathophysiologies and that the mouth and the gut form part of the same mucosal tract but provide numerous microhabitats to host specific consortia of bacteria. Both are subject to epithelial ulceration in response to underlying inflammatory-immune responses to emergent dysbiosis within their microbiota.
The dental team as part of the healthcare team
The links between periodontal disease and systemic health issues mentioned above are only a sampling of the many that have been observed and studied. This data and research underscore the need to reconsider a dentist’s role in the health and well-being of their patients. Many people tend to think of oral care as distinct and separate from overall well being, but as we can see, this is not the case.
Sharing this information with patients, in a way that is intended to inform and encourage good oral care rather than scaring or causing a panic, can be extremely helpful toward solidifying ritualistic habits, strong relationships, and ultimately better health outcomes.
The power of prevention in periodontal disease
It all comes back to the incredible value of strong preventative measures for oral health. The number one way to keep periodontal disease and inflammation at bay is by adhering to a consistent and proper care routine that involves brushing at least twice daily, cleaning interdentally between the teeth, and regularly visiting the dentist or dental hygienist for check-ups and supportive therapy.
Oral care professionals can take the extra step of learning about their patients’ general health background, and offering additional guidance, information, and encouragement for those who might be at any heightened risk for the above systemic issues.
At SUNSTAR GUM®, we offer a wide assortment of products that help everyone keep their mouths and bodies healthy.




















