
New Research Offers Guidance on Partnering with Patients for Lifelong Periodontal Care
Periodontal treatment is needed to address periodontitis issues for patients. But as any dental professional knows, the treatment itself is rarely enough to resolve the disease for good.

Ongoing care from both patient and dentist are critical to ensuring long-term success for almost any surgical or non-surgical treatment, and avoiding relapses.
New research makes it clearer than ever that participation from both sides is essential. A key challenge, and opportunity, for dental professionals today is to build strong supportive periodontal care programmes.
Here’s what you should know.
Periodontal maintenance vs. supportive periodontal therapy
Throughout most of the industry, post-treatment periodontal care is divided into two categories:
- Maintenance therapy: referring more to the patient’s role.
- Supportive therapy: referring more to that of the practitioner.
The European Federation of Periodontology (EFP) has defined guidelines around best practices for this post-treatment phase of care. These documents note that many patients remain at high risk for recurrence or progression, due to continuing gingival inflammation and/or a lack of regular follow-up care.
The EFP recommends “specifically designed supportive periodontal care (SPC), consisting [of] a combination of preventive and therapeutic interventions rendered at different intervals which should [include]: appraisal and monitoring of systemic and periodontal health, reinforcement of oral hygiene instructions, patient motivation towards continuous risk factor control, professional mechanical plaque removal (PMPR) and localized subgingival instrumentation at residual pockets.”
The guidelines go on to emphasise the importance of a structured recall system for professional interventions.
“This step should be rendered at regular intervals according to the patient’s needs, and in any of these recall visits, any patient may need re‐treatment if recurrent disease is detected, and in these situations, a proper diagnosis and treatment plan should be reinstituted.”
“In addition,” the EFP adds, “compliance with the recommended oral hygiene regimens and healthy lifestyles are part of supportive periodontal care.”
These two cornerstones of supportive periodontal care – regularly scheduled recall sessions, and proactive patient self-maintenance – go hand in hand, with new evidence showing that practitioners may need to consider a more active position in this relationship.
Developing a sustainable supportive periodontal care programme
A recently published study by Bittencourt et al. aimed to investigate the effectiveness of patient self-responsibility in periodontal care after professional treatment. The results were not encouraging, showing a high rate of regression to pre-treatment conditions and thus leading the researchers to conclude:
“Self-responsibility for the continuation of periodontal care after professional treatment should be avoided.”
For dependable success in supportive periodontal care, a long-term programme with ongoing frequent recalls should be highly encouraged by clinicians and specialists.
The reality is that patients often waver over time in their commitment to post-treatment maintenance.
There is a natural tendency to turn attention elsewhere, and thus discontinue prioritisation of the proper care or continued appointment-setting. Practitioners should strive to impress upon their patients the importance of lifelong supportive periodontal care, and how ongoing adherence to the programme significantly reduces likelihood of future complications or treatments.
Ultimately, no matter how much adentist oral care professional cares or tries, there is no ability to directly control the actions or mentality of a patient. However, we can try to influence our patient’s behaviour.
The best we can do is take an active role as partners and advocates, clearly spelling out the facts and risks, while remaining empathetic to the fact that it can feel harder for patients to build mental urgency around continued maintenance for a treatment that may have taken place multiple years ago. Establishing shared goals, working together on a planning, and scheduling regular recurring visits to monitor progress are essential.
Continue reading to learn what recall interval is recommended.
Putting a SPC programme plan in place
According to EFP recommendations, “supportive periodontal care visits should be scheduled at intervals of 3 to a maximum of 12 months and ought to be tailored according to patient's risk profile and periodontal conditions after active therapy.” A review in 2020 by Trombelli et al determined that, “In patients affected by moderate to advanced periodontitis, a supportive periodontal therapy protocol based on a 2-4 month recall interval appears reasonable.”
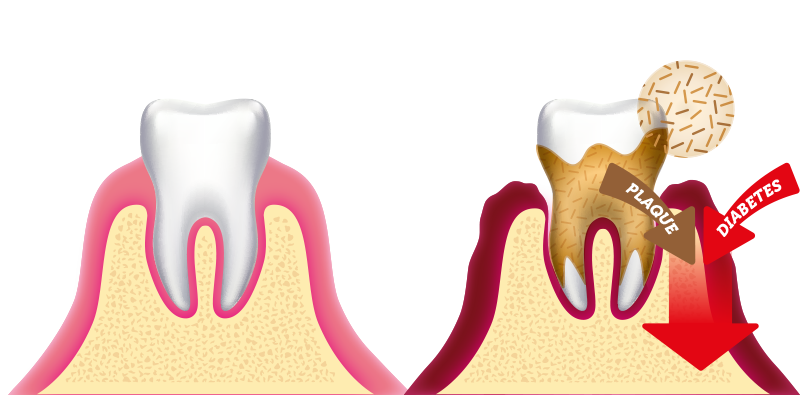
In addition to clinical actions during visits, such as appraisal of periodontal health and PMPR, dentists should use these engagements as key opportunities to clarify oral hygiene instructions and reinforce patient motivation – specifically with regards to continuous risk factor control, such as tobacco smoking cessation and diabetes control interventions – and by using behavioural change techniques.
Advances in dental technology and practitioner technique have elevated periodontal treatments to new levels, with amazing results that can last a lifetime – but only if both dentist and patient are ready to play a lasting, consistent role in sustaining those results.
How do specialists in periodontology deal with such challenges? What type of solutions do they have at their disposal, and what are their strategies in daily practice? Let’s hear it from two renowned experts in the field and check out the video below on periodontology and home-based oral care.

