
Periodontitis, Diabetes, and Dental Implants: An Overview
SUNSTAR has been actively supporting research into diabetes for over three decades, inspired by founder Kunio Kaneda’s personal battle with diabetes. While Kaneda ultimately passed away prematurely due to diabetic complications, his family and the organisation he founded continue to honour his legacy through their work.
Let’s look at what some of this research has revealed about the link between diabetes and periodontitis, as well as its impact on implant complications.

Characteristics and prevalence of diabetes and periodontitis
In recognition of World Diabetes Month, Sunstar and the Spanish Society of Periodontology (SEPA) invited Prof. Filippo Graziani to host a webinar on the bidirectional relationship between diabetes (type 1 and 2) and periodontitis.
Read on for key insights and highlights on this topic.
Diabetes
Diabetes is a metabolic disorder marked by disrupted metabolism and excessive levels of glucose in the bloodstream. This is the result of insufficient insulin secretion and/or insulin resistance, as insulin is the hormone that is responsible for the uptake of glucose from the bloodstream into the cells.
- Type 1 diabetes is caused by a deficiency in insulin secretion that results in elevated levels of glucose in the bloodstream.
- Type 2 diabetes is caused by impaired insulin receptors. While the body produces insulin, the defect in receptors leads to insensitivity to insulin, sometimes called insulin resistance.
Both of these conditions result in a state of hyperglycemia, which is defined by blood glucose levels above 125 mg/dL and glycated haemoglobin, HbA1c, above 6.5%.
Patients with diabetes are at higher risk of developing significant complications, such as cardiovascular diseases, stroke, kidney failure, retina problems, and neuropathy, which can lead to amputations of extremities, mainly the foot (also called diabetic foot).
According to the most recent data from the World Health Organization (WHO), the prevalence of diabetes has risen dramatically over the past 40 years, now affecting roughly 9% of the global population. This figure is expected to reach double digits by 2045.
Periodontitis
Periodontitis is the chronic progression of untreated gingivitis. It is characterised by inflammation, bone loss, and recession of the gums. In the latest classification of periodontal diseases, there are four stages and three grades of periodontitis, with grades B and C containing indicators related to diabetic progression.
The disease's peak incidence is between 30-40 years, and it can lead to tooth loss and edentulism, which adversely affects the patient's social, psychological, and overall health.
The WHO estimates that “severe periodontal diseases are estimated to affect around 19% of the global adult population.”
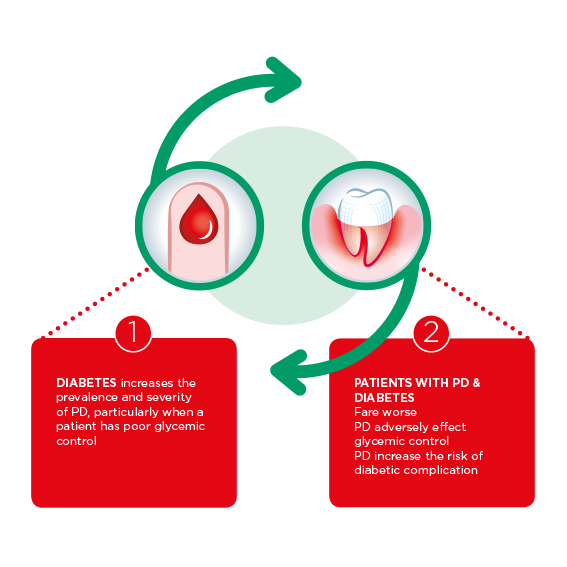
The bidirectional relationship between diabetes and periodontitis
The link between diabetes and periodontitis has been known for well over 25 years. In that time, studies have revealed that each disease increases the risk of developing the other.
Diabetic risk factors for periodontitis
Individuals with uncontrolled type 2 diabetes are three times more likely to develop periodontitis (Shlossman et al, 1990), and have four times the risk of alveolar bone loss (Taylor et al. 1998) and a greater incidence of tooth loss (Demmer et al 2012) when compared to patients with controlled diabetes.
These earlier findings were validated by the more recent work of Sanz et al 2017, whose consensus report by the International Diabetes Federation and the European Federation of Periodontology concluded that “there is strong evidence that people with periodontitis have elevated risk for dysglycaemia and insulin resistance.”
There is evidence that suggests the level of control patients have over their diabetes is a significant factor in developing periodontitis. One study (Tsai et al., 2002) found that “individuals with poorly controlled diabetes had a significantly higher prevalence of severe periodontitis than those without diabetes (odds ratio = 2.90; 95% CI: 1.40, 6.03), after controlling for age, education, smoking status, and calculus. For the better-controlled diabetes subjects, there was a tendency for a higher prevalence of severe periodontitis (odds ratio = 1.56; 95% CI: 0.90, 2.68).”
The pathogenic mechanisms that link periodontitis and diabetes include:
- Changes in the microbiota of patients with poorly controlled diabetes. Research (Polak & Shapira, 2017) indicates that in patients with poorly controlled diabetes, there is a change in the microbial composition of dental plaque towards perio-pathogens.
- Alteration of immune cell functions. Subjects with both type 1 and type 2 diabetes and periodontitis exhibit a greater propensity for local inflammation, with a larger proportion of inflammatory molecules (interleukins 1β, 4, 7, and prostaglandins) present in the gingival crevicular fluid than those with periodontitis alone.
- The production of Advanced Glycation End products resulting from hyperglycemia is linked to increased alveolar bone destruction and altered wound healing.
Periodontal risk factors for diabetes
Prof. Graziani’s own research (Graziani et al. 2017) reveals that non-diabetic individuals with periodontitis “exhibit a poor glycaemic control and a higher risk of developing diabetes,” by as much as 29% within 5 to 13 years.
It was also found that individuals with both periodontitis and diabetes experience more complications, particularly diabetic retinopathy and cardio-renal diseases, compared to those with diabetes alone. The severity of periodontitis directly correlates with the presence of microalbuminuria or end-stage renal diseases in both type 1 and type 2 diabetes patients.
Individuals with diabetes and periodontitis have a 3.5 times greater risk of dying from cardiorenal problems than those with diabetes only. In subjects with type 1 and type 2 diabetes, periodontitis increases the overall mortality and cardiovascular mortality over 14 years. In nondiabetic patients, periodontitis leads to higher levels of HbA1c, fasting blood glucose, and increased diabetes prevalence.
The ulcerated tissues caused by periodontitis result in a higher influx of bacteria in the bloodstream and an elevated level of systemic inflammation. These bacteria may colonise atheromatous plaques and facilitate their rupture, leading to cardiovascular and metabolic diseases. Additionally, periodontitis is associated with alterations in the metabolism of high-density lipoproteins, dysvitaminosis, adipocyte alterations, and oxidative stress, ultimately exacerbating diabetes by elevating HbA1c levels.
How diabetes affects dental implant patients
A 2022 study by Nibali et al. examined implant complications in diabetic patients with a history of periodontitis to answer the question: can diabetics get dental implants? Because chronic periodontitis can lead to alveolar bone loss and tooth loss, the treatment of periodontitis may require dental prostheses, such as dental implants.
This meta-analysis found that patients who have a history of periodontal disease are at a higher risk of developing peri-implantitis, compared to those without a history of periodontitis (Ong et al., 2008). When uncontrolled diabetes is also a factor, it negatively impacts osseointegration. However, patients with controlled diabetes experienced osseointegration (Javed and Romanos, 2009).
Another significant finding of the Nibali et al. study was that “uncontrolled diabetes, together with genetic predisposition, smoking, history of periodontitis, specific subgingival microbes, and residual subgingival cement are generally considered as predisposing to peri-implant diseases,” concluding that implant therapy is not recommended for patients who do not have their diabetes under control.
Effects of periodontitis treatment on diabetes
Patients with controlled diabetes can expect to respond to periodontitis treatment the same as patients without diabetes. However, diabetic patients who do not have their diabetes under control will typically show a higher recurrence of periodontal pockets than their controlled counterparts.
The followings studies have documented the effectiveness of periodontitis treatment on glycemic control in diabetic patients:
- D’Aiuto et al., 2018 found that periodontitis treatment in patients with diabetes reduces HbA1C by 36%, stating that “routine oral health assessment and treatment of periodontitis could be important for effective management of type 2 diabetes.”
- Genco and Borgnakke, 2020 showed improved glycemic control in type 2 diabetes among patients receiving treatment for periodontitis. A secondary benefit for patients was a lower incurment of medical costs each year.
- Graziani et al. 2015 found that subjects undergoing a full-mouth approach to periodontitis treatment had significantly higher levels of acute inflammation within the first 24 hours compared to those undergoing conventional treatment.
Prof. Graziani noted that antibiotics are not necessary to treat subjects with periodontitis.
A recent study was published by SUNSTAR and the University of Buffalo (Li et al, 2023) that offered new insights into periodontits treatment options for patients with type 2 diabetes. The purpose of the study was to evaluate the effects of an intensive, at-home, chemical, and mechanical antiplaque regimen, as well as study the results of this treatment among patients with type 2 diabetes and nondiabetics. The study found that chemo-mechanical antiplaque measures may improve outcomes in subjects with diabetes after nonsurgical periodontal therapy.
Recommended institutional actions
Common guidelines around the treatment of periodontitis in patients with diabetes were drawn up during the 2018 meeting of the European Federation of Periodontology with the International Diabetes Federation and supported by SUNSTAR.
These guidelines are:
- Doctors treating diabetic patients should conduct inspections of any oral symptoms and refer patients to the dentist for treatment, as well as a yearly oral screening.
- Dentists should discuss the impact of periodontitis with their diabetic patients, and patients with periodontitis should be referred to a doctor for diabetes screening.
- Patients with both diabetes and periodontitis should immediately receive a non-surgical treatment. Surgery and implant are possible if the diabetes is controlled.


