
Obesity and Periodontal Disease: What Your Patients Should Know
Obesity is a global epidemic that anybody working in the field of health and medicine is dealing with. According to the World Health Organization, the worldwide obesity rate has tripled since 1975, with some 13% of adults categorized as obese.

The condition is strongly linked to cardiovascular disease, diabetes, and other significant health consequences.
In the dental community, professionals are invested in understanding the links between inflammatory periodontal disease and systemic health conditions, and obesity is a prevalent focus. The relationship between obesity and periodontal disease is a growing area of study.
Let’s explore some of the latest research on this topic, so you can keep your patients informed and vigilant.
Understanding obesity
Body weight can be a sensitive topic for anyone, so it’s always best to approach it from a scientific, fact-based place. The diagnosis of obesity is based on Body Mass Index (BMI), a value defined as body weight divided by the square of body height. For adults, a BMI that is equal to or greater than 30 qualifies as obese. (Greater than or equal to 25 qualifies as overweight.)
A frequent underlying driver of obesity is metabolic syndrome, which is not a distinct disease on its own but rather a grouping of risk factors including high blood pressure, high blood sugar, unhealthy cholesterol levels, and abdominal fat. Metabolic syndrome has its own documented relationship with periodontitis but for the purposes of this article we’ll be mostly examining the link with obesity specifically.
The links between periodontitis and obesity
Over the years, various studies have been conducted to better understand the relationship between these two multifactorial chronic inflammatory diseases.
In a 2018 study by Suvan et al., the meta-analysis of 14 systematic reviews concluded that “obese individuals are more likely to have periodontal diseases, with more severe periodontal conditions, than nonobese individuals.”
“Because obesity may contribute to periodontal complications independently of other risk factors”, the authors said, “there is a need for risk assessments for individual patients to facilitate personalized approaches in order to prevent and treat periodontal diseases.”
Two years later, in 2020, Jepsen et al. published a paper on the association of periodontal diseases with metabolic syndrome and obesity, noting that, “Extensive research has established plausible mechanisms to explain how these conditions can negatively impact each other, pointing to a bidirectional adverse relationship... The global burden of periodontitis combined with the obesity epidemic has important clinical and public health implications for the dental team.”
Most recently, a 2021 study from the University of Buffalo attempted to explain the mechanistic link between these two conditions in greater detail. “Chronic inflammation caused by obesity may trigger the development of cells that break down bone tissue,” researchers found.
Specifically, it is suggested that excessive inflammation resulting from obesity increases MDSC (myeloid-derived suppressor cells) quantity as part of the body’s immune response. These MDSCs, originating from bone marrow, develop into a range of different cell types, including osteoclasts, that break down bone tissue and lead – in the oral region – to alveolar bone loss. This could explain how “obesity – by inflating growth of bone-destroying cells – raises the risk of periodontal diseases.”
Obesity and diabetes in the scope of oral care
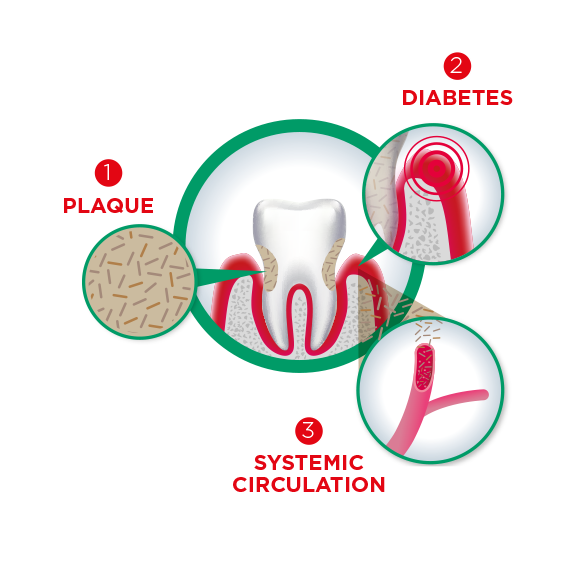
In the past we’ve discussed the association between periodontal diseases and diabetes. This is important to consider with regard to obesity and periodontitis, considering the strong links between diabetes and obesity.
In short, obesity is one of the major risk factors for insulin resistance, resulting in impaired glucose levels with diabetes as an end-point. According to research, obesity is believed to account for 80-85% of the risk of developing type 2 diabetes, with obese individuals being up to 80 times more likely to develop type 2 diabetes than those with a BMI of less than 22.
In addition, an expansive new tooth loss study sponsored by SUNSTAR found clear evidence that poor glycemic control for people over 30 resulted in fewer natural teeth. As preventing tooth loss is an imperative priority for dentists and their patients, this insight can heavily influence conversations around the urgency of oral care, especially for those who might be at greater risk.
As such, dental professionals should account for the matter of obesity and glycemic control when communicating to their patients about their oral health implications and vice-versa. Our whitepaper on diabetes, gum health, and periodontal disease features a wealth of information to help guide these dialogues.
Advise patients about dental risks of obesity and diabetes
As with many other links between periodontal disease and systemic health issues, this one serves as a reinforcing message around the vital importance of strong oral care, especially for patients who might be experiencing, or are at heightened risk for, these conditions.
In addition to providing a clear and compelling course of action to help patients take control of their at-home oral care, you may consider some specific lifestyle recommendations that also address the issue of obesity. For example, advising patients around nutrition and gum disease, to show that many dietary choices that positively impact oral health are also beneficial for controlling glycemic levels and reducing BMI.
Additionally, encourage physical activity that contributes to holistic health. A recent study published in JAMA Internal Medicine, for example, found that “cycling was associated with lower all-cause and CVD mortality risk among people with diabetes independent of practicing other types of physical activity. Participants who took up cycling between the baseline and second examination had a considerably lower risk of both all-cause and CVD mortality compared with consistent non-cyclists.”
Oral health is intrinsically linked to obesity and diabetes just as those two conditions are linked to one another. Understanding the broader relationship between all three helps patients take control of their overall health and drive toward better outcomes, in the mouth and beyond.
