Oral Health in the Time of COVID-19
Oral Care Professionals have been identified as one of the highest-risk groups for contracting the 2019-nCoV virus. The postponement of all elective dental procedures has been widely recommended to help mitigate the spread of COVID-19. For dental practices, what are the recommendations when delivering unavoidable emergency procedures?

For our patients, how can viral infection interact with pre-existing periodontitis? How can we support during the Coronavirus pandemic?
Viral infection and periodontal disease: what do we know and what can you do to help your patients?
Viral infection and periodontal disease: what do we know? Not much, says Professor Graziani, Professor of Periodontology at the University of Pisa (Italy) and Past President of the European Federation of Periodontology (EFP). But we do know that oral health is as important as ever, he adds.
From the basic science perspective and from our experience with HIV, we know that poor oral health may lower the defenses of mucous membranes and make epithelial cells more susceptible to viruses [1].
“Significantly, some herpes family viruses may be associated with some forms of gingival inflammation, including Herpes Zoster, Cytomegalovirus and the Epstein-Barr virus (EBV)”, Professor Graziani explains. “While we do not know much about these viruses’ impact on oral health, they may have a role in moving or triggering a lesion to progress from gingivitis to periodontitis, or they may co-participate to some deterioration”.
It is also well established that oral infection and especially periodontitis affects the course and pathogenesis of systemic diseases, including cardiovascular disease and diabetes mellitus. Bad oral health also has a negative impact on the pathogenesis of bacterial pneumonia [2] which in a COVID-19 patient would result in the co-existence of bacterial and viral infection in the respiratory tract, complicating remission.
For all of these reasons, recommending good oral health practices to all patients is as important as ever during the COVID-19 pandemic.
How can we help patients cope? Let your patients know that maintaining good oral health should be part of their ‘stay healthy’ strategy during COVID-19. This is particularly important for patients living with diabetes or any other patient known to you that has comorbidities that are known to be COVID-19 risk factors.
Dentists are a high-risk group. Medical societies recommend undertaking emergency procedures only
Dental practices are exposed to a tremendous risk of 2019-nCoV infection due to the face-to-face communication and the exposure to saliva, blood, and other body fluids, and due to the handling of sharp instruments, warn two recent publication in the International Journal of Oral Science and in the Journal of Dental Research [3] - [4]. Indeed, as the Italian experience shows, health care workers are the category with the highest diffusion of 2019-nCoV contagion [5].
Throughout the world, dental associations have provided guidance and made recommendations to their members. Given the fast changing nature of the pandemic, the advice is continuously evolving and influenced by updates from the World Health Organization (WHO), National Health Ministries and local medical organizations. The associations who have made recommendations to their members are too numerous to enumerate, but include the DZB German Dental Association [6], the British Dental Association [7], the Spanish Dental Association (Consejo General de Dentistas de EspañaI [8], the American Academy of Periodontology [9], and the American Dental Association [10] and more.
The key recommendations are to treat only emergency procedures as per definitions and guidelines provided by the local professional societies and health ministries.
How to reduce risk of person-to-person transmission during emergency procedures?
Recommendation for infection control measures in dental clinics and hospitals have been made to limit the person-to-person transmission routes.
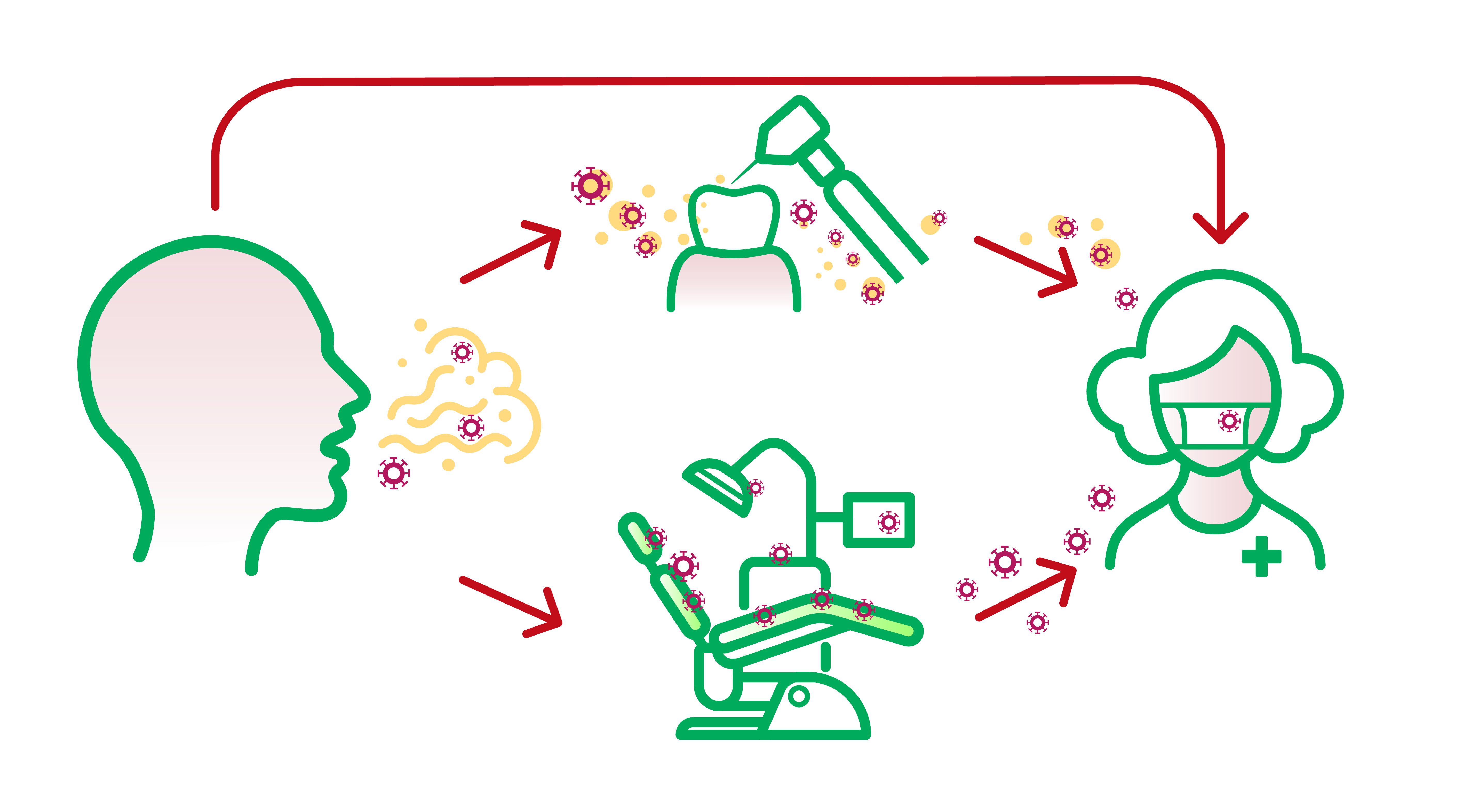
Adapted from Peng, Peng, Xian et al “Transmission routes of 2019-nCoV and controls in dental practice” International Journal of Oral Science (2020).
Evaluating patients with COVID-19
Dental professionals may find themselves in a position of having to identify a suspected case of COVID-19. Adequate testing capacity for SARS-CoV-2 is lacking worldwide. The WHO is continually updating technical guidance for COVID-19, including recommendations on laboratory testing.
According to the latest report in the Journal of Medical Virology [11], a statistical analysis of the clinical symptoms and laboratory results of COVID-19 patients identifies the following incidence of clinical symptoms:
- Fever (88,5%)
- Cough (68,6%)
- Myalgia or fatigue (35,8%)
- Expectoration (28,2%)
- Dyspnea (21,9%).
Minor symptoms include headache or dizziness (12,1%), diarrhea (4,8%), nausea and vomiting (3,9%).
On April 1, a team at King's College London looked at responses from more than 400,000 people reporting suspected COVID-19 symptoms to an app and found that loss of smell and taste could also be a symptom COVID-19 [12]. However, loss of smell and taste are also signs of other respiratory infections such as the common cold, so the jury is still out on whether this potential symptom is of practical relevance.
Patient Triage
For treatments that cannot be postponed, all dental practitioners are advised to mandatorily perform phone triage to define the real need for emergency treatment i.e. treatment of acute pain, abscesses, trauma, and hemorrhagic events. Dentists are then encouraged to organize patients flux in order not to have more than one patient in the waiting room [5].
Pre-procedural use of mouth rinses
A pre-procedure antimicrobial mouth rinse is generally believed to reduce the number of oral microbes, even if chlorhexidine, which is commonly used as mouth rinse in dental practice, may not be effective to kill 2019-nCoV [2].
According to the Chinese experience, since 2019-nCoV is vulnerable to oxidation, pre-procedural mouth rinse containing oxidative agents such as 1% hydrogen peroxide or 0.2% povidone is recommended instead. It is hoped that this would help reduce the salivary load of oral microbes, including potential 2019-nCoV.
Rubber dam isolation
The use of rubber dams can significantly minimize the production of saliva- and blood-contaminated aerosol or spatter, particularly in cases when high-speed hand pieces and dental ultrasonic devices are used. Use of rubber dam isolation is therefore recommended during the COVID-19 epidemic [2] - [4].
Anti-retraction hand piece
The high-speed dental hand pieces without anti-retraction valves may aspirate and expel the debris and fluids during the dental procedures. More importantly, the microbes, including bacteria and viruses, may further contaminate the air and water tubes within a dental unit, and thus potentially contribute to cross-infection.
Peng, Xian et al. found that anti-retractive valves or other anti-reflux designs for dental handpieces can instead significantly reduce the backflow of oral bacteria and HBV as compared with the handpiece without anti-retraction function. These are therefore recommended as an extra preventive measure against cross-infection [2].
Radiography
Intraoral x-ray examination can stimulate saliva secretion and coughing and is therefore not recommended during the COVID-19 outbreak [4]. Extraoral dental radiographies, such as panoramic radiography and cone beam CT, are recommended instead.
Disinfection of the clinic settings and management of medical waste
Strict disinfection measures in both the clinic settings and in the public waiting area are highly recommended.
Medical waste generated by the treatment of patients with suspected or confirmed 2019-nCoV infection should be regarded as infectious medical waste, and should be treated as such according to best practice in each country.
Convalescing patients
While it was reported that non emergency dental care should be postponed at least 1 month for convalescing patients with SARS, it is currently unknown yet whether the same suggestion should be recommended for patients with COVID-19 [4].
Operative checklist summary
For a convenient operative checklist for dental practitioners during COVID-19, see summary recommendations by Professor Graziani’s team developed in consideration of both the Chinese and the Italian experience [5].
Key take-aways
- Oral Care Professionals have been identified as one of the highest-risk groups for contracting the 2019-nCoV virus. Treat only emergency patients.
- For our patients, this is good time to remind them that good oral health is part ‘stay healthy’ strategy during COVID-19. Poor oral health may lower the defenses of mucous membranes and make epithelial cells more susceptible to viruses.
- Recommendation for infection control measures in dental clinics have been made and other than disinfection procedures include anti-retraction hand pieces, rubber dam isolation, and pre-procedural 1% hydrogen peroxide or 0,2% povidone mouthrinses.



